Anal Cancer Screening Guidelines for PLHIV
Last updated: November 2024
Methods
Populations to screen
Globally, PLHIV experience the highest incidence of ASCC2. Despite the benefits for the health of PLHIV, studies have shown that ART has not led to a reduction in the incidence of anal HSIL or anal cancer among PLHIV4-19. The extraordinarily high incidence of ASCC in PLHIV has become more evident due to improved access to ART and increased longevity in PLHIV20-21.
Studies from the past two decades have shown that among PLHIV, the highest ASCC incidence was found among GBM with HIV (85 per 100,000). Women living with HIV (WLHIV) have an incidence of between 18.6 and 35.6 per 100,00022-23. A recently published systematic review and meta-analysis of cancer risk in PLHIV found ASCC had a standardised incidence ratio of 37·28 (95% Confidence Interval 23·65–58·75)24. These incidence rates are mostly greater than the incidence of cervical cancer among the general female Australian population prior to the introduction of widespread cervical Pap screening in 1991, which was 18 per 100 000 person years25.
Understanding ASCC incidence by age is essential to inform potential screening programs. A nationwide data linkage study to identify cancer diagnoses in PLHIV was conducted in Australia between 1982 and 2012, demonstrated that the incidence of anal cancer in PLHIV aged between 35 and 64 years has increased significantly over the past three decades5. The age-standardised incidence of anal cancer per 100,000 person-years in three age groups, and overall, is shown in Table 1.
Table 1. Annual age-standardised anal cancer incidence per 100,000 by overall and by three age groups in PLHIV in Australia, from 1982 to 2012
| 1982-95 | 1996-99 | 2000-04 | 2005-08 | 2009-12 | p-value* | |
|---|---|---|---|---|---|---|
| Overall | 26.82 | 18.76 | 25.40 | 38.41 | 44.97 | 0.002 |
| Age (years) | ||||||
| 15-34 | 4.41 | 12.40 | 0.00 | 4.55 | 4.34 | 0.621 |
| 35-64 | 24.49 | 16.99 | 41.13 | 41.69 | 66.44 | <0.001 |
| > 65 | 84.83 | No cases | 34.86 | 105.22 | 71.43 | 0.553 |
A sub-group of the IANS guidelines taskforce undertook a literature review and meta-analysis of ASCC incidence in groups at established elevated ASCC risk, to evaluate ASCC incidence estimates by risk group and age (Figure 1)26. Eight studies reported ASCC incidence rates in PLHIV, with the largest contribution from the US HIV/AIDS Cancer Match study (Table 3). The overall incidence rates per 100,000, by risk group, were 85 (95% Confidence Interval (CI) 82-89), 32 (95% CI 30-35) and 22 (95% CI 19-24) for GBM, non-GBM males and females, respectively. The data were further stratified by age group (Figure 1)26.
In relation to PLHIV being followed-up after treatment for anal cancer, data from the United Kingdom (UK) have reported the detection of HSIL in 13% of all patients after chemoradiation and 74% of all patients after excision only, supporting the need for careful surveillance to detect and treat HSIL among this population with a history of ASCC, particularly following surgical excision27 28. PLHIV with previously diagnosed HSIL, for example during an unrelated procedure such as haemorrhoidectomy, colonoscopy or through anal tissues samples taken to investigate other anal pathologies should also be screened regularly for residual HSIL, new HSIL and anal cancer with HRA29-30.
Figure 1. Anal cancer incidence per 100000 person years, by gender, age and risk group
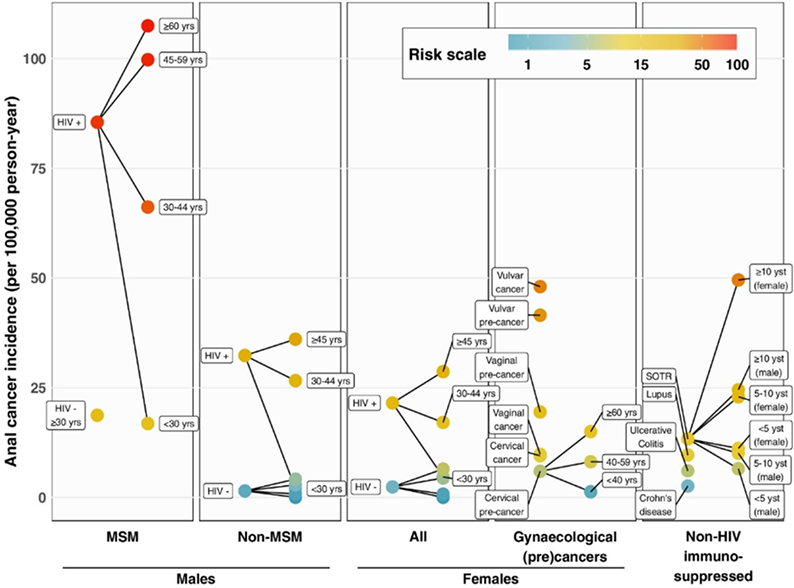
In the US HIV/AIDS Cancer Match study, the risk of anal cancer increased exponentially from age 30 years and above, in all populations (Table 2)26
Table 2: Age-specific anal cancer incidence in PLHIV, U.S. HIV Cancer Match study, 1996-2015
| HIV Risk Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| MSM | Non-MSM Males | Females | |||||||
| Age group (years) | Cases | Person-years | IR per 100,000 person-years (95% CIs) | Cases | Person-years | IR per 100,000 person-years (95% CIs) | Cases | Person-years | IR per 100,000 person-years (95% CIs) |
| < 30 | 32 | 190,168 | 16.8 (11.5-23.8) | 2 | 99,327 | 2.0 (0.2-7.3) | 7 | 150,038 | 4.7 (1.9-9.6) |
| 30-44 | 533 | 805,573 | 66.2 (60.7-72.0) | 131 | 492,496 | 26.6 (22.2-31.6) | 91 | 532,692 | 17.1 (13.8-21.0) |
| 45-59 | 695 | 696,830 | 99.7(92.5-107.4) | 246 | 674,139 | 36.5 (32.1-41.3) | 136 | 458,248 | 29.7 (24.9-35.1) |
| > 60 | 123 | 114,467 | 107.5 (89.3-128.2) | 49 | 144,168 | 34.0 (25.1-44.9) | 19 | 82,520 | 29.7 (24.9-35.1) |
The IANS consensus guidelines taskforce categorised the meta-analysis ASCC incidence estimates into two groups. Risk Category A included high-risk groups with an incidence of at least 17 per 100,000 (defined as at least 10-fold greater incidence compared with the general US population incidence of 1.7 per 100,000 person-years). All PLHIV groups were included in this category. The taskforce developed specific recommendations for age of commencement of screening for PLHIV, determining that screening should begin at age 35 years in GBM and trans women and at age 45 years for women with HIV and non-GBM men.
ASHM’s age-based recommendation for ASCC screening corresponds with both the IANS and DHHS guidelines.
Resources
Legal
About Us
Contact Us
ASHM Head Office – Sydney
Level 3, 160 Clarence Street Sydney, NSW 2000
Tel: (+61) 02 8204 0700 Fax: (+61) 02 8204 0782
![]()
![]() Acknowledgement of Country
Acknowledgement of Country
ASHM acknowledges the Traditional Owners of Country across the various lands on which we live and work. We recognise Aboriginal and Torres Strait Islander peoples’ continuing connection to land, water, and community and we pay our respects to Elders past and present. ASHM acknowledges Sovereignty in this country has never been ceded. It always was, and always will be, Aboriginal land.
ASHM Health | ABN 48 264 545 457 | CFN 17788 | Copyright © 2024 ASHM

